Giving Poultry a Healthy Start
You would think vaccinating poultry against avian influenza (AI) would be a good thing, given that the last major U.S. outbreak in 2014-2015 directly cost the federal government and producers $3.3 billion and the overall cost to the U.S. economy was even higher by the time it was all over.
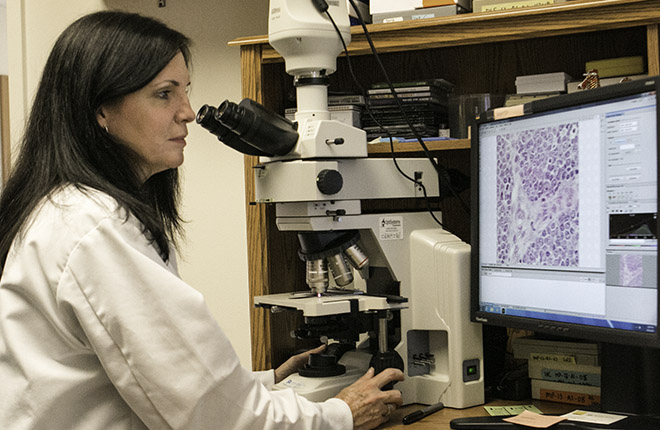
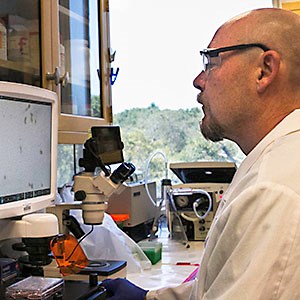
However, relying on vaccines to prevent or control AI outbreaks in this country is a very complicated issue, explains David Suarez, research leader of the Agricultural Research Service (ARS) Exotic and Emerging Avian Viral Diseases Research Unit in Athens, Georgia, part of the U.S. National Poultry Research Center. There, ARS conducts work on AI, including evaluating existing vaccines, especially against new strains, and developing improved vaccine production methods and better ways to administer them.
For an AI vaccine to work well, it has to match the specific strain of virus causing the outbreak, and there may be only limited cross-protection between strains, Suarez explains.
|
|
AI viruses are initially categorized by their ability to cause disease symptoms. Those that cause few or no clinical signs in infected birds are labeled low pathogenic (low path). The more virulent form is classified as highly pathogenic (high path). Then, strains are further subdivided by their combination of two groups of proteins found on the surface of the virus: hemagglutinin proteins (H), of which there are 16 (H1–H16), and neuraminidase proteins (N), of which there are 9 (N1–N9).
While low-path AI rarely poses a serious threat to either humans or the U.S. poultry industry, some low-path strains can mutate into the more highly pathogenic forms.
The designation of low path or high path is based on a specific test in poultry and does not provide any information about the potential virulence of AI viruses in humans.
Each time birds appear to be sick or to have died from AI, samples are taken and shipped to the U.S. Department of Agriculture (USDA) Animal and Plant Health Inspection Service (APHIS) National Veterinary Services Laboratories (NVSL). That lab provides the official diagnosis, determines whether the virus involved is high or low path, and “serotypes” the virus—identifies its H and N proteins—and at least partially sequences the virus’s genome. Important viruses are then shared with ARS labs for additional analysis.
With an identification in hand, the ARS lab evaluates existing commercial vaccines against that particular strain to see if any provide adequate protection.
“We routinely evaluate existing vaccines against new and emerging AI virus strains as they appear around the world, so we always have a pretty good idea of where we are covered and where new vaccines may be needed in order to offer poultry the best protection,” says Suarez. “But when we receive a sample from a sick bird in the United States that could signal an outbreak involving a new strain, that’s when the lab really shifts into high gear.”
That’s exactly what happened in December 2014, at the beginning of what would become the largest AI outbreak ever in domestic and wild birds in the United States. Within weeks, Suarez and other ARS scientists had developed a molecular test that could quickly and specifically distinguish the new virus (a high-path Asian H5) from low-path North American viruses. Today that type of test, called “real-time RT-PCR,” is used during AI outbreaks in the United States and many other countries to provide sensitive, specific identifications in as little as 3 hours.
Next, the lab tested the six vaccines then commercially available for H5 AI viruses against this new strain—only to find that none adequately protected chickens.
“We weren’t surprised to find there wasn’t enough protection,” Suarez says. “Our research had shown that AI vaccines only have a lifespan of about 2 to 4 years before they won’t work well enough against circulating virus strains.”
|
|
Then, the lab’s entire team worked swiftly to develop a new seed vaccine to match the high-path H5N2 and H5N8 viruses that were causing the 2014-2015 outbreak. Using a technique called “reverse genetics,” researchers were able to manipulate the viruses’ genes to take the hemagglutinin gene from its high-path sequence and modify it into a matching low-path virus. The modified influenza virus, which was still a perfect match to the field strain, allowed for safer production of the vaccine with no chance of spreading a high-path virus during a potential vaccination program.
ARS transferred the seed vaccine to a commercial company for large-scale production. More than 50 million doses of the new vaccine were added to the National Veterinary Stockpile, where they could potentially be used as a tool in future outbreaks if necessary.
AI viruses also mutate very quickly. They are RNA viruses—meaning the virus has RNA inside, but no DNA; RNA is less stable, Suarez explains. As RNA mutates, it makes changes in the surface proteins to which the vaccine binds, like a key into a lock. Enough changes—about 2 years’ worth—and the key may no longer fit the lock.
Suarez and his colleagues have also done studies that indicate vaccination in birds may hasten the genetic drift that makes the vaccines obsolete. “We think vaccine use provided a selective pressure for new variations of the virus to emerge and become the dominant circulating strain,” Suarez explains. “Using vaccines means you need to do more field monitoring to detect when viruses diverge from the vaccine.”
In addition to speeding up vaccine development, ARS is also looking for faster and easier ways to administer vaccines. Injecting poultry one by one is too slow and labor intensive to help in an outbreak, even as a last resort.
There are practical ways to mass vaccinate poultry, such as spraying the vaccines. But spray vaccination involves operators entering each poultry house with backpack-mounted devices, increasing the opportunity for pathogen spread. Some trials have found that as few as 30 to 60 percent of birds in a house are fully vaccinated by this method.
Vaccines can also be added to poultry drinking water. But that too can lead to contamination problems, and it can be hard to track whether each bird receives the vaccine.
 Chickens get vaccinated by a prototype automated vaccine delivery system ARS developed. (Joseph Purswell, D3868-1)
|
Veterinarian Scott Branton and agricultural engineer Joseph Purswell with the ARS Poultry Research Unit at Mississippi State, Mississippi, have developed a fully automated vaccinating system that could overcome these issues. The system uses changes in lighting to trigger birds to drink from water lines. While the birds drink, strategically placed nozzles descend from the ceiling and spray the birds with vaccine. The specific target is the eye area, where vaccines are easily absorbed. The vaccine can also be picked up through preening and contact with other birds.
“We tested our prototype against a three-person crew with backpack sprayers in a large commercial laying operation,” Branton says. “We used a vaccine for infectious bronchitis and Newcastle disease. The birds in the houses with our automated system had a higher rate of complete vaccination with better protection, as measured by higher levels of circulating antibodies to these diseases.”
Purswell adds, “As we refined the system and got more experienced using it, we started getting a 100-percent success rate in having birds vaccinated. And we did it faster and with fewer people.”
The automated vaccine delivery system has been patented and licensed to the Long Branch Company Inc., West Point, Mississippi, which has already installed two systems. One of those is in the layer houses of Cal-Maine Foods, Jackson, Mississippi, the largest producer of shell eggs in the United States. Their total flock is about 36 million layers and 9.5 million pullets and breeding chickens.
Other Countries
While several other countries, especially Mexico, Indonesia, China, Vietnam, and Egypt, depend heavily on vaccinating chickens, ducks, and other poultry to keep HPAI viruses in check, in the United States, eradication has been the response of choice. This means when high-path AI is found in domestic birds, APHIS orders a culling or depopulating of the entire infected flock and certain flocks in close proximity. Because the virus is highly contagious and easily spread in poultry, buildings and equipment are rigorously disinfected before new birds are allowed back, a process that takes at least several weeks.
“Some countries use billions of doses of AI vaccines as a way of controlling high-path outbreaks by preventing clinical disease, but they are not getting rid of the virus,” Suarez says. “In the United States, we typically eradicate every time the virus shows up in domestic birds, and we don’t vaccinate anything for high-path AI.”
There’s another reason for not vaccinating U.S. chickens: Many countries impose import restrictions on trade of poultry and poultry products if vaccine is used in a control program. USDA believes that if vaccines were used, it could cost U.S. producers billions in trade revenue. The United States is the world’s largest producer and exporter of poultry. In 2016, total U.S. poultry exports including eggs reached $4.65 billion, according to the U.S. Census Bureau.
During the 2014-2015 AI outbreak, 18 countries blocked imports of any American poultry or eggs, and another 38 countries blocked imports from the states that specifically had AI problems.
Until there are vaccines that can successfully address all of the issues, APHIS will continue to hold vaccination as a tool of last resort—something to turn to only if an AI outbreak spreads beyond what depopulating can control. Only then will APHIS call for zones of vaccination to be done around centers of depopulation in hopes of stemming the outbreak.—By J. Kim Kaplan, ARS Office of Communications.
Key Facts
- Avian influenza (AI) viruses can cost producers billions of dollars in losses.
- Using AI vaccines is complicated, since viruses mutate quickly.
- Existing vaccines may not protect poultry against new virus strains.
- ARS developed a seed vaccine and an automated vaccination system that provides better AI protection.
Full Story